Background on Antimicrobial Resistance
Antimicrobial resistance (AMR) is a growing concern in healthcare settings worldwide. It refers to the ability of microorganisms, such as bacteria, viruses, and fungi, to evolve and become resistant to the drugs that were previously effective in treating them. This rise in resistance poses a significant threat to human health, causing difficulties in managing infections and increasing the risk of complications.
According to the World Health Organization (WHO), AMR is one of the top 10 global public health threats facing humanity. It affects the effective treatment of conditions like urinary tract infections, bacterial infections, bloodstream infections, skin infections, and respiratory infections.
The Centers for Disease Control and Prevention (CDC) estimates that each year in the United States alone, at least 2.8 million people acquire antibiotic-resistant infections, leading to more than 35,000 deaths.
This problem arises due to the misuse and overuse of antibiotics in humans and animals, as well as the lack of development of new antimicrobial drugs. In addition, the spread of resistant infections within healthcare facilities, also known as hospital-acquired infections (HAI), further exacerbates the issue.
Addressing antimicrobial resistance requires a multifaceted approach, including infection control and prevention practices, antibiotic stewardship programs, and improved surveillance and diagnostic techniques. With the continued rise of resistant bacteria, it is crucial for healthcare workers and public health departments to stay informed and vigilant in combating this global challenge.
AMR’s Impact on Healthcare Workers
As the world grapples with the growing threat of AMR superbugs, healthcare workers face several challenges in their line of duty. These risks include:
1. Increased incidence of drug-resistant infections: The rise of AMR has led to an alarming increase in drug-resistant infections, making it more challenging for healthcare workers to effectively treat patients. This puts them at a higher risk of encountering infections that do not respond to conventional antibiotic treatments.
2. Occupational exposure: Healthcare workers are at a heightened risk of exposure to drug-resistant pathogens due to their close proximity to infected patients. This exposure can occur through direct contact, respiratory droplets, or contaminated surfaces, making healthcare settings potential hotspots for the spread of AMR superbugs.
3. Transmission to vulnerable populations: Healthcare workers, unknowingly carrying drug-resistant bacteria, can inadvertently transmit these organisms to vulnerable populations such as elderly patients, newborns, or individuals with compromised immune systems. This can result in severe and life-threatening infections in already susceptible individuals.
4. Limited treatment options: With the rise of AMR, the arsenal of effective antibiotics is dwindling. Consequently, healthcare workers may face limited treatment options when dealing with drug-resistant infections, making it harder to provide effective care and potentially prolonging recovery times for patients.
5. Occupational burnout and stress: The challenges posed by AMR and the increased workload associated with managing drug-resistant infections can lead to higher levels of occupational burnout and stress among healthcare workers. This can impact their well-being and patient care outcomes.
6. Inadequate infection prevention and control strategies: Healthcare facilities must implement rigorous infection prevention and control strategies. However, the rise of AMR superbugs poses a unique challenge in maintaining effective measures, potentially increasing the risk of healthcare-associated infections.
Hospitals’ Role in Preventing AMR Spread
Hospitals must take proactive measures to protect staff and patients to minimize the spread of drug-resistant infections. Here are some impactful strategies employed by hospitals to prevent the spread of antimicrobial-resistant superbugs:
1. Strong infection control protocols:
- Implementing strict hand hygiene practices among healthcare workers.
- Utilizing personal protective equipment (PPE) such as gloves, gowns, and masks when appropriate.
- Practicing proper cleaning and disinfection of medical equipment and surfaces.
2. Enhanced surveillance and monitoring:
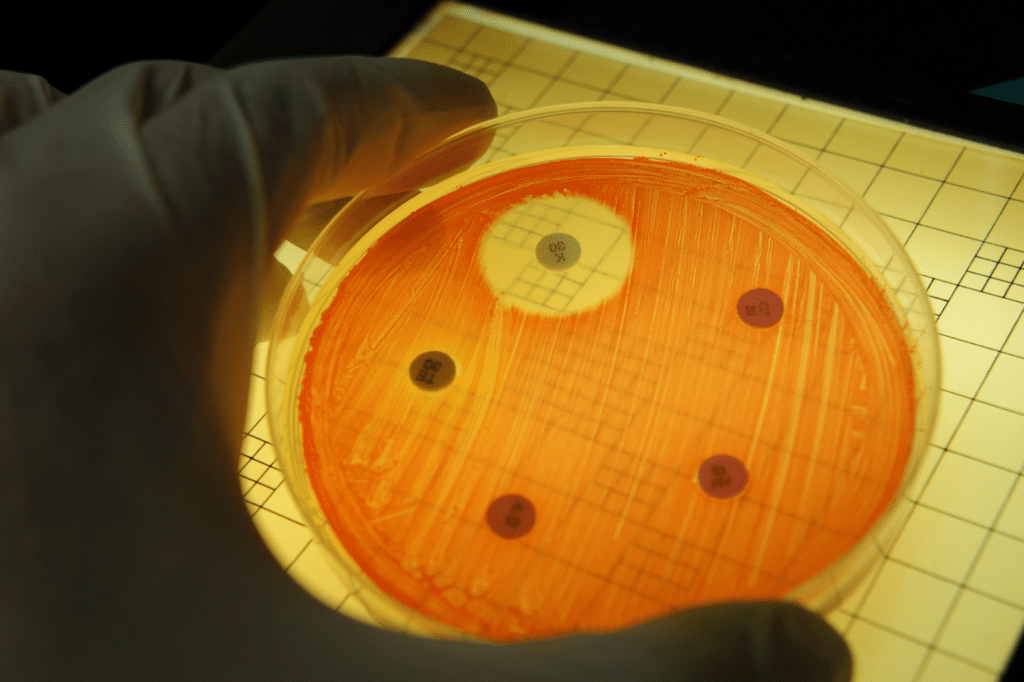
- Conducting regular surveillance to identify resistant bacteria and track their prevalence.
- Utilizing infection preventionists to monitor and analyze infection data.
- Implementing effective communication systems to promptly notify healthcare staff of any outbreaks or clusters.
3. Antibiotic stewardship programs:
- Promoting responsible and judicious use of antibiotics through education and guidelines.
- Encouraging the use of appropriate antibiotic treatment duration and dosage.
- Adopting strategies to ensure timely review, reassessment, and streamlining of antibiotic therapy.
4. Screening and isolation measures:
- Identifying patients colonized or infected with resistant bacteria through active screening.
- Implementing isolation precautions, such as placing affected patients in single rooms or cohorting.
- Adhering to established transmission-based precautions for contagious pathogens.
5. Education and training:
- Educating healthcare workers on the importance of AMR and proper infection control practices.
- Conducting regular training sessions to enhance staff knowledge and skills.
- Ensuring clear communication channels to address queries and concerns related to AMR.
Hospitals play a crucial role in preventing the spread of antimicrobial-resistant superbugs. These proactive measures not only protect the health and well-being of individuals but also contribute to the overall fight against antimicrobial resistance.
Future Outlook of Antimicrobial-Resistant Superbugs
Experts warn that healthcare workers and hospitals can expect AMR spread challenges to persist in the coming years. And with the rise of antimicrobial resistance, there is a limited arsenal of effective antibiotics available.
Healthcare workers may face challenges in finding suitable treatments for certain infections. As these infections become harder to treat, patients may experience longer hospital stays, more severe illness, and increased mortality rates.
Healthcare workers will need to prioritize infection prevention and control practices to limit the spread of superbugs. This includes robust hand hygiene, proper sanitation, and adherence to isolation precautions.
Experts also emphasize the importance of collaboration between healthcare providers, public health agencies, and researchers to address this issue. Sharing knowledge and developing strategies collectively will be crucial in combating antimicrobial resistance.
National Action Plans for Reduce AMR Spread
Several countries around the world have developed National Action Plans (NAPs) to address the growing concern of AMR. These plans aim to reduce the spread of AMR, increase awareness, improve surveillance, and implement strategies to ensure the appropriate use of antimicrobial drugs. Here are a few examples of implemented NAPs:
1. United States National Action Plan on Combating Antibiotic-Resistant Bacteria (CARB): This plan focuses on slowing the emergence of resistant bacteria, strengthening surveillance efforts, improving antibiotic stewardship, and advancing research to develop new antibiotics and diagnostics.
2. United Kingdom Five-Year Antimicrobial Resistance Strategy: The UK’s plan focuses on improving infection prevention and control practices, optimizing prescribing practices, promoting research and development, and enhancing international collaboration to tackle AMR.
3. Australian National Antimicrobial Resistance Strategy 2015-2019: This strategy prioritizes the education of healthcare professionals and consumers, strengthening surveillance systems, promoting innovation, and improving infection prevention and control practices in healthcare settings.
4. The Netherlands National Action Plan on Antimicrobial Resistance: This plan aims to reduce the inappropriate use of antibiotics, promote research and development, strengthen surveillance systems, and foster international cooperation to combat AMR.
These NAPs, along with many others implemented worldwide, provide a comprehensive framework to address antimicrobial resistance.
By combining different strategies and interventions such as infection control, surveillance, education, and research, these plans aim to mitigate the spread of AMR and preserve the effectiveness of antimicrobial drugs for future generations.
Overall, the outlook on antimicrobial-resistant superbugs is challenging for hospitals, but not hopeless. Do all that you can to be aware and proactive in the fight against AMR spread.From a PPE perspective, HAI challenges like this are what we made Sloan Medical’s PPE for. If you have not requested a free sample of our gowns, booties, or other protective equipment, please take advantage of our free offers now.