In hospitals and long-term care facilities, infection control is everyone’s responsibility. Amidst the rise of drug-resistant microbes, we all need to stay informed about the latest developments in health care-associated infections.
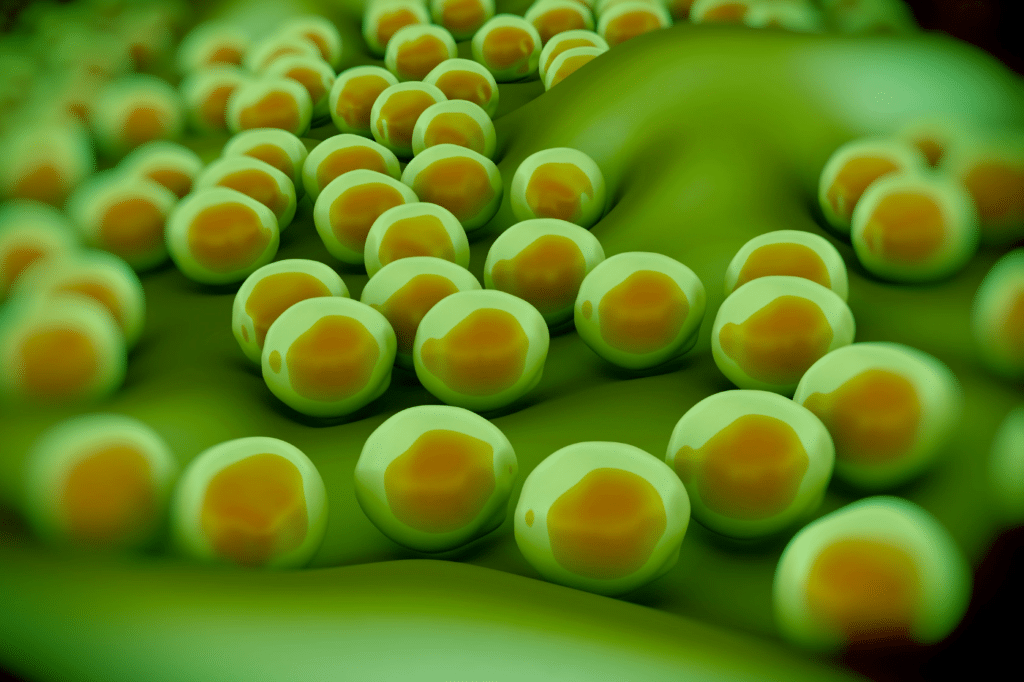
One concerning trend we’re seeing is the rise of drug-resistant fungal infections in healthcare settings. These resilient fungi pose a significant threat to the well-being of healthcare workers and patients alike. Are facilities adequately prepared to combat these formidable adversaries?
The emergence of drug-resistant fungi has become a pressing issue in the healthcare industry. As the use of antifungal medications has increased, so too have cases of resistance, leaving healthcare workers scrambling for effective treatment options. The consequences of these drug-resistant fungi can be dire, leading to prolonged hospital stays, increased healthcare costs, and even fatalities.
As healthcare workers continue to battle against these tenacious fungi, it is crucial to understand the key strains that pose the greatest threat. By identifying the top drug-resistant fungi, we can better equip ourselves with the knowledge and resources needed to protect both healthcare workers and patients from their potentially devastating effects. In this article, we will explore the most concerning drug-resistant fungi and the steps being taken to combat this growing threat.
Why are fungal infections increasing?
In 2019, the U.S. Centers for Disease Control and Prevention estimated that 18 superbugs—both drug-resistant fungi and bacteria—cause at least 2.8 million drug-resistant infections every year in the United States, resulting in more than 35,000 deaths (2). (ncbi.nlm.nih.gov)
There are several reasons for the increase in fungal infections, including:
Climate Change:
Changes in temperature and humidity levels can create the perfect environment for fungi to thrive and spread. As the climate becomes warmer and more humid, the conditions become more favorable for fungal growth.
Antibiotic Use:
Overuse and misuse of antibiotics can lead to an imbalance in the body’s natural flora, making it easier for fungi to take hold and cause infections.
Weakened Immune Systems:
Patients with weakened immune systems, such as those with HIV/AIDS, cancer, or diabetes, are more susceptible to fungal infections. Intensive Care Unit patients are particularly vulnerable.
As the population ages and more individuals are living with chronic illnesses, the risk of fungal infections increases. Antifungal drugs are only so effective, and these urgent threats can’t be ignored. Prevention is a powerful ally in this fight.
Healthcare professionals need to be aware of these factors and take proactive measures to prevent fungal infections in their patients. This includes proper hand hygiene, environmental cleaning, appropriate use of antifungal medications, and the proper use of PPE.
One of the most important ways to keep patients and staff safe from drug-resistant fungal infections is the use of impermeable personal protective equipment (PPE.) This includes wearing gloves, gowns, boot and shoe covers, aprons, masks, and eye protection when necessary, and following proper donning and doffing procedures. Patients should be protected from cross-contamination through the use of disposable patient transfer sheets and mattress covers.
By staying informed and implementing effective infection control measures, we can work together to combat the increasing prevalence of fungal infections in the United States.
Fungi of greatest concern
According to the Centers for Disease Control and Prevention, numerous fungi pose the greatest concern in the United States. The following are the key fungi causing infections at an alarming rate:
– Candida auris
– Aspergillus fumigatus
– Cryptococcus neoformans
– Histoplasma capsulatum
These drug-resistant strains are of particular concern due to their ability to cause severe and sometimes life-threatening infections, especially in individuals with weakened immune systems.
Candida Auris, for example, is a multi-drug resistant yeast that has caused outbreaks in healthcare settings. Aspergillus fumigatus can lead to invasive aspergillosis, a serious infection that primarily affects the lungs. Cryptococcus neoformans and Histoplasma capsulatum are known for causing severe respiratory infections, especially in those with compromised immune systems.
Even healthy people can fall prey to fungal infections. Health care facilities must be vigilant in preventing the spread of these fungi, particularly in healthcare settings where vulnerable individuals may be at greater risk of infection, such as long-term care facilities, nursing homes, and hospitals.
Candida auris: An Emerging Drug-Resistant Fungal Threat
Of special note is the emerging threat of Candida auris (C. Auris) infection. This drug-resistant fungal infection poses a serious threat in health care facilities and the patients we care for.
The statistics are grave:
- C. auris now kills 30% to 60% of patients with bloodstream infections (8). (ncbi.nlm.nih.gov)
- The number of fungal infections reported as the cause of death steadily increased in the United States between 2013 and 2018, from 4,000 to about 5,000, according to one longitudinal analysis (3). (ncbi.nlm.nih.gov)
C. Auris reached New York, New Jersey, and Illinois last year, leading the federal Centers for Disease Control and Prevention to add it to a list of germs deemed “urgent threats.” The deadly, drug-resistant fungus is infecting patients in hospitals and nursing homes around the world. Source: nytimes.com
C. Auris infection is especially concerning for a few reasons:
– Difficult to treat: C. Auris is resistant to many antifungal medicines, making it challenging to treat. This can lead to antifungal resistance in your patient population.
– Healthcare-associated infections: This pathogen can spread rapidly in healthcare settings, leading to outbreaks and increased risk for vulnerable patients.
– Serious complications: C. Auris infections can lead to serious complications, including bloodstream infections and invasive infections of organs.
Healthcare workers must remain vigilant in their infection control practices to prevent the spread of C. Auris in their facility. This includes:
– Strict adherence to hand hygiene protocols
– Utilizing appropriate personal protective equipment
– Implementing environmental cleaning and disinfection protocols
– Conducting surveillance for early detection of C. Auris cases
By staying informed and proactive, we can work together to mitigate the threat of C. Auris and ensure the safety of the patient population.
What can the medical community do?
As with most things in medicine, an ounce of prevention is worth a pound of cure. Preventing the spread of drug-resistant fungal infections in healthcare settings is much easier than treating staff and patients once infected.
Take a look at your facility’s infection control procedure, and ensure that all PPE products meet or exceed the ASTM’s F1671 test standards. Truly impermeable, disposable personal protective equipment (PPE) for staff and patients can make all the difference.
We recommend two key prevention tips:
– Using disposable patient transfer sheets and mattress sheets to prevent cross-contamination between patients.
– Using PPE boot covers, jumpsuits, and aprons that meet the ASTM’s F1671 test standards.
Investing in premium PPE that meets these high standards will protect both patients and healthcare workers from the spread of drug-resistant fungal infections. By ensuring that PPE is impermeable and meets specific test standards, we can effectively prevent the spread of fungi in healthcare settings.
Infection prevention is everyone’s responsibility. Nurses and staff always prioritize the safety and well-being of our patients. Facilities can support nurses in this mission by carefully selecting and consistently supplying the highest quality impermeable PPE available.
Designed by Healthcare Professionals, for Healthcare Professionals
Available exclusively through Sloan Medical, STA-DRI garments and ezGLIDE® disposable patient transfer sheets were designed for healthcare professionals by urologist Dr. Stewart Sloan.
We strive to keep surgeons and nurses safe during patient care and surgeries. Our PPE garments are designed to be lightweight, durable, and—yes—impenetrable. All our products meet or exceed ASTM’s F1671 test standards. This test method is used to measure the resistance of materials used in protective clothing to penetration by pathogens.
We’re so confident you’ll love our products that we’ll send you a sample for free. Fill out this form to get started.